First-in-Human T1D Vaccine Trial Reports Positive Results
Wouldn’t it be nice if you could take a vaccine as a child—like you do for mumps, polio, and measles—and type 1 diabetes (T1D) would not develop? This could be a real option for families in the not-too-distant future.
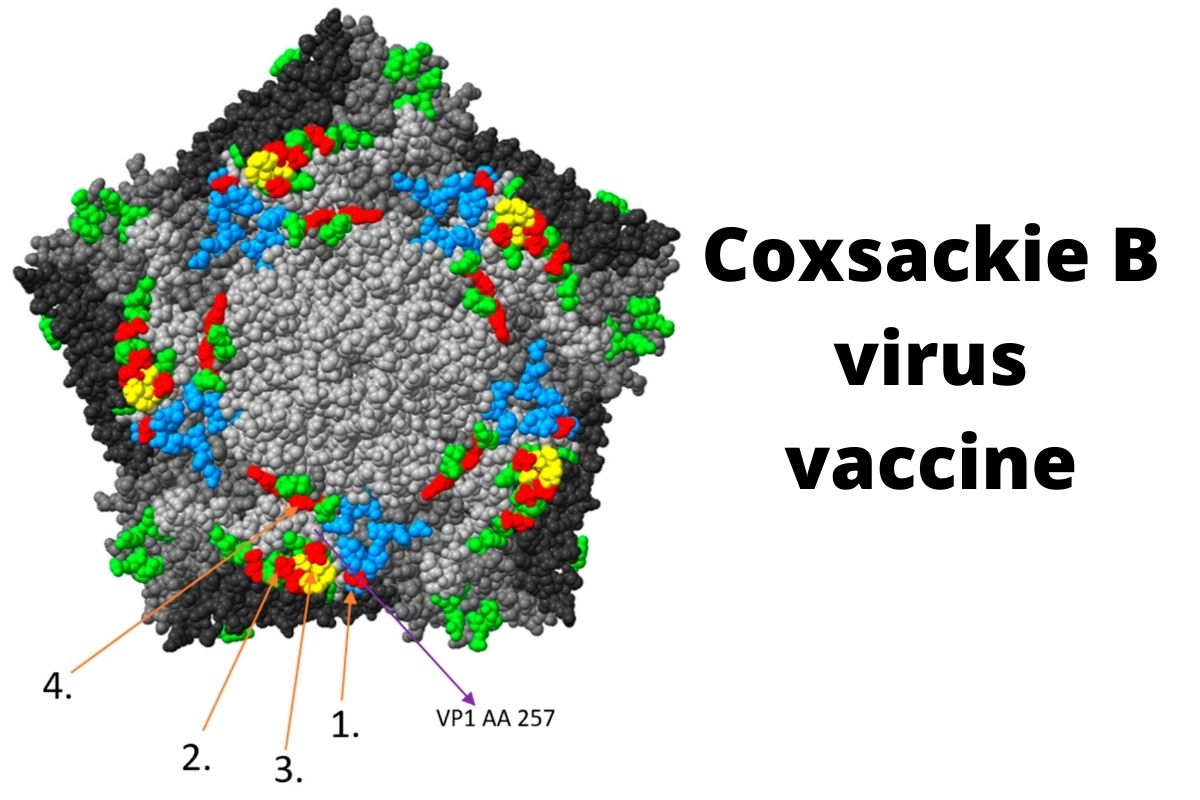
The viral hypothesis posits that a viral infection may be partly responsible for T1D. The main culprit appears to be coxsackie B—a common pathogen where, in most circumstances, the infection is asymptomatic or results in mild symptoms. (Coxsackie B, however, in rare cases, may also lead to viral meningitis, heart or brain infection, and hand, foot, and mouth disease.)
There have been no vaccines against coxsackie B, until a year ago, when the company Provention Bio started a clinical trial to test its vaccine against coxsackie infection.
This is a first-in-human study of PRV-101, and positive interim results are out. Not only was it well tolerated, but it induced high concentrations of anti-coxsackie B antibodies.
A JDRF Story
JDRF has been studying viral vaccines for T1D for decades, and so has the JDRF T1D Fund, our venture philanthropy started in 2016:
- JDRF has been funding viruses in the development of T1D since the late 1970s and demonstrated that several common viruses known to infect humans can attack islet cells and induce symptoms resembling diabetes. But what virus? Mumps, Epstein-Barr, rubella?
- In 1994, JDRF funded a postdoctoral fellowship for Heikki Hyöty, M.D., Ph.D., working in the lab of Michael Knip, M.D., Ph.D. The project title: “The Role of Coxsackie B and Other Enteroviruses in the Pathogenesis of Insulin-Dependent Diabetes Mellitus.” He went on to show that enteroviruses—of which coxsackie B is a member of—are the main culprit for the development of T1D. We have gone on to fund Dr. Hyöty with more than 10+ grants since, and Dr. Knip with more than 20 grants since 1997.
“One of the most critical steps was a postdoctoral grant I received from JDRF in 1994. This grant made it possible to continue in science instead of clinical work, which I was considering at that time. I established my own research group, studying the role of virus infections in T1D, and have continued this work since then.”
– Heikki Hyöty, M.D., Ph.D.
- Hyöty and Knip co-founded Vactech in 2001, who developed PRV-01, a vaccine candidate targeting coxsackie B virus, and licensed it to Provention Bio in 2017.
- In 2017, Provention Bio* got an investment from the JDRF T1D Fund, to get their coxsackie B vaccine into clinical trials, the start of which happened in December 2020.
Next Steps
This was only the interim results; the final results will be revealed next year. But, if they are the same as the interim results, continued development of the vaccine and its use to reduce the burden of T1D will be under way.
This vaccine is the result of decades’ long support from JDRF and is part of the many approaches JDRF is taking to create a world with T1D. Will you join us?
*Provention also has teplizumab, the first drug to delay the onset of T1D for nearly 3 years, under review by the FDA. JDRF had a hand in the development of teplizumab from almost the beginning. We gave a Career Development Award to Kevan Herold, M.D., who had just started his faculty-level career at The University of Chicago, in 1988-1990. He showed, in an early animal study, that he could prevent autoimmune diabetes with an anti-CD3 antibody (which, later, became a humanized version, teplizumab). He has gone on to receive more than 15 grants from JDRF, and was the lead on the clinical trial that demonstrated that it could delay the onset of T1D for nearly three years.
Citation: Honkimaa A, Kimura B, Sioofy-Khojine AB, Lin J, Laiho J, Oikarinen S, Hyöty H. Genetic Adaptation of Coxsackievirus B1 during Persistent Infection in Pancreatic Cells. Microorganisms. 2020 Nov 15; 8 (11): 1790. doi: 10.3390/microorganisms8111790.