Participation in Clinical Trials

NIH link participating in clinical trials
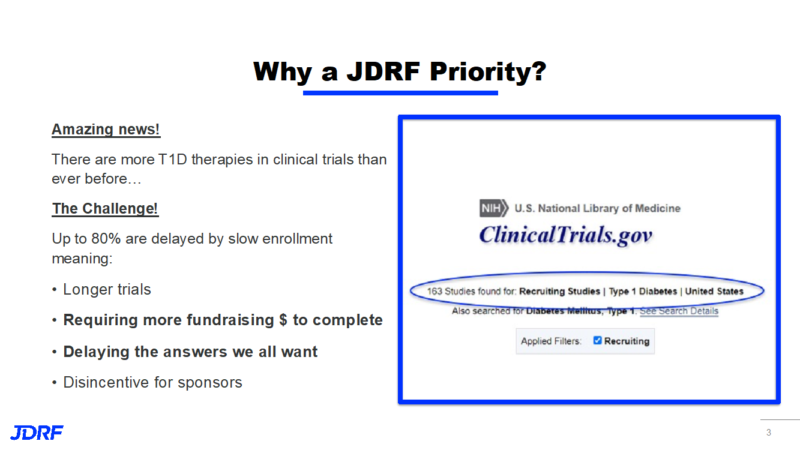
JDRF is successful in accelerating research discoveries and is currently funding over 70 clinical trials. A clinical trial is a carefully designed study in which a participant may take a new drug or use a new treatment that may allow researchers to answer a specific medical question. Examples of questions researchers are trying to answer are: does it improve a medical condition?; will it have side effects?; what is the dose that is effective?; and is it a better treatment than what is currently being prescribed per the Standard of Care?. A clinical trial is the most important last step before a new treatment or new device can apply for FDA approval and become available to the public. Currently clinical trials on prevention, new treatments, and cures are delayed when there are not enough people to participate in trials. Our JDRF Minnesota and Dakotas chapter is fortunate to have several research institutions, and therefore around 26 clinical trials, available for adults and pediatric T1D participants. TrialNet is a large study for those genetically susceptible to developing T1D, with the goal of preventing T1D before it becomes clinical T1D. Minnesota and Dakotas Chapter trials currently cover prevention and cure, trials for those newly diagnosed with T1D, an encapsulation device trial for those with hypoglycemia, and trials for complications of T1D.
There are many reasons to consider participating in a clinical trial, which include:
• It is through clinical trials that new drugs, therapies, and ultimately a cure for T1D will be discovered.
• You may get a new treatment for a disease before it is available to the general public.
• You play a more active role in your own healthcare.
• Researchers may provide you with medical care and more frequent health check-ups as part of your treatment.
• Devices and new medications that are part of the trial are covered – this offers access to pumps and CGMs you normally don’t have.
• You may have the chance to help others get a better treatment for their health problems in the future.
• You keep your current doctor.
• You can stop participating at any time if new concerns arise, or if you lose your confidence that the potential benefit outweighs the risk.
Read more about clinical trials from the National Institute of Health (link to expand).
Currently when you are prescribed a treatment by a doctor in their office, this is called the Standard of Care. The Standard of Care is a care plan that has been tested and approved, and works for most people. Clinical trials test potential treatments in human volunteers to see whether they should be approved for wider use in the general population, and whether they provide better outcomes for a disease. A treatment could be a drug, medical device, biologic, or behavioral intervention. Clinical trials are conducted only after health and ethics committees, such as the IRB (see below), have given their approval for the trial. Each trial has a certain number of participants that are required. This number is important for the validity and efficacy of the trial. It is also important to have a diverse group as it applies to age, gender, and ethnicity. Differences within these groups may show different responses to the disease being studied along with treatments being tested. Treatments having acceptable safety profiles and showing promise are then considered for a phase 2 or 3 clinical trial. The phase 1 trial is the initial safety trial involving a small number of participants (20-100 individuals). It is not uncommon in a trial that the treatment being used is a treatment commonly used for another disease. This means the drug may have a lengthy safety track record of many years. Researchers continue to study treatments after they have been approved. These trials often involve large numbers of participants. They continue to follow these participants and check to see if the treatment works well over time.
The team working on answering a research question in a clinical trial consists of the Principal Investigator (PI) and the Clinical Research Coordinator (CRC) or the Study Coordinator. Consider the PI to be like a head coach, as they are responsible for leading the trial, formulating the design of the study (such as randomization), as well as recording and analyzing all of the data. The PI develops the study protocol, which is the set of instructions that everyone on the team must follow carefully. The CRC or Study Coordinator is like the assistant coach who works alongside the PI. They will handle all of the day-to-day activities and will be the main contact for those who volunteer to participate in a clinical trial. They are also the individuals that can provide you with a wealth of information about any details of the clinical trial, such as how long it lasts, risks and benefits, and what your responsibilities are as a participant. This is all covered in a document called “informed consent”. Informed consent is designed to answer all of these questions and is required by the FDA and local ethics committees. Informed consent is a very important part of any clinical trial and is an ongoing process during a trial. Before you can participate in a trial, you must read, understand, and sign the informed consent form. You have the right to understand the purpose, benefits, risks, and side effects of the clinical trial along with the right to stop participation.
The Institutional Review Board (IRB) is a board that provides volunteer protections for those participating in a clinical trial. The IRB’s role is to make sure a trial is ethical, fair, safe, and not too risky. The IRB receives continual updates during a trial and must be notified of any serious side effects from study drugs or interventions that may require a change in the study plan. The IRB can stop a trial if it feels volunteers are not safe.
In previous surveys by JDRF, those who have participated in a clinical trial are often likely to participate in additional trials after they finish their current trial. In a 2017 survey, 91% of clinical trial participants said they would “definitely” or “probably” recommend clinical trial participation to friends or a family member. Inquiring about a clinical trial gives the study staff at the research institution the opportunity to explain all facets of the trial and for you to ask questions. This first step does not mean you have to sign up for the trial you are asking about. It helps to make that initial call or to send an email and gather the information you need in order to know more about the trial.
I am the Clinical Trial Education Volunteer (CTEV) for our JDRF Minnesota and Dakotas Chapter. If you need help with the JDRF connection tool, clinicaltrials.gov, or have other questions about clinical trials/studies in general, I would be glad to answer your questions. I can be reached at debbieaevans1@gmail.com or 612-810-1933.
As you look at descriptions of trials in your area, the contact person such as the CRC or Study Coordinator can best answer questions specific to the trial of interest.