JDRF is the leading global organization harnessing the power of research, advocacy, and community engagement to advance life-changing breakthroughs for type 1 diabetes (T1D). Learn More
Early Symptoms of T1D
What to look for in infants/toddlers, children, teens, and adults.
T1D FAQ
What is type 1 diabetes? Can it be prevented? How is it managed?
The Latest
Slowing the Progression of T1D
Results Are Out: Tzield Benefits Newly Diagnosed Individuals
Learn More
T1D Screening and Monitoring
Learn why you should be screened, how to get screened, and what to do with your results.

Activate Change: Become a JDRF Advocate
Champion federal funding for T1D research. Inform health and regulatory policy. Improve lives.

All About Clinical Trials
Find out why more people need to participate and how to find a clinical trial near you.
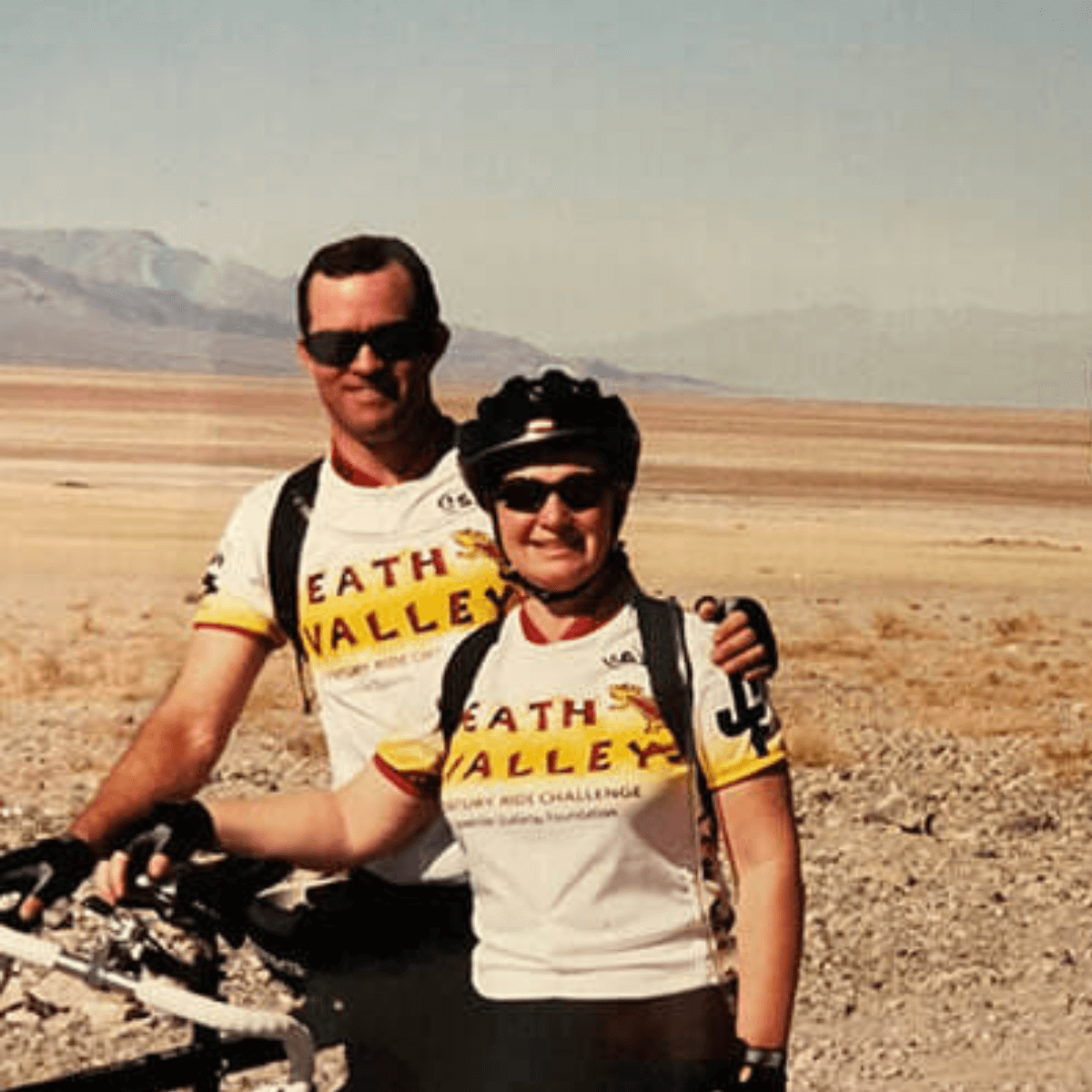
Still Riding After All These Years
The Roettkers have been JDRF Ride participants since the beginning, pedaling thousands of miles to end T1D. For them, it's not just about the miles—it's about the mission.

Advancing on many fronts
JDRF is the world’s largest nonprofit funder of type 1 diabetes research. Our in-house scientists oversee a diverse portfolio of research tracks, leaving no stone unturned in our search for a cure.
Learn More about Advancing on many fronts
Improving lives, today and tomorrow
While our focus is on curing type 1 diabetes (T1D), we also pursue new treatments to keep people with T1D healthy until that day comes. Outside of the lab, we push for increased government funding for research, and work with academia, clinicians, insurers and regulators to get new therapies and devices to market quickly and safely.
Learn More about Improving lives, today and tomorrowType 1 Diabetes Resources
Connect with others or find useful guides for navigating some of the trickier moments of life with type 1 diabetes (T1D).
JDRF One Walk®
Our biggest event of the year is a fun way to connect with people in your area who understand what it’s like to live with T1D, while raising money and awareness. Walk on your own, or register with your family, friends, classmates or colleagues.
Find a WalkWant more ways to connect with your community? JDRF hosts a variety of events year-round, including golf tournaments, galas, summits, support groups, research opportunities and rides.
See All Events Near You
Coverage 2 Control
JDRF’s experts partner with our volunteers across the nation to advocate for affordability, choice, and coverage of the T1D therapies that work best for you.
Health Insurance: Explained
In addition to assistance with cost of insulin, JDRF’s T1D Health Insurance Guide helps families navigate topics including prior authorizations, denials and appeals, and applying for an exception.
Learn moreYour gift today gets us a step closer to a world without T1D.












