Inside a T1D Clinical Trial: A NorCal Teen’s Perspective
by Brody Paine, 17
Four years ago, when my primary care doctor told me that I didn’t have time to run home and prepare for a multi-day hospital visit before meeting an endocrinologist in the emergency room, my family and I were very worried to say the least. Prior to a routine visit, I presented nearly every symptom of undiagnosed type 1 diabetes (T1D) but the drowsiness, thirst, and weight loss blended right in with a combination of puberty, growing, covid protocols, and zoom “school”. My mother expressed concern about my symptoms in a letter my father and I took to the doctor. The doctor immediately checked my blood sugar, saw that it was ~450 mg/dl following a bowl of Cinnamon Toast Crunch, and sent me on my “merry” way to the ER in San Francisco.
 During my extended hospital stay, I learned all about my diagnosis from how my pancreas decided to indefinitely go on strike to why that black and white table on the back of food boxes is actually really important. Between seeing the diabetes educator, endocrinologist, and amazing nurses, I met a JDRF rep who gave me a care package of everything a newly diagnosed T1D teen may need. Most notably, a teddy bear with highlighted fur of where I should and should not stick needles into myself. Also included in the JDRF care package was a reference sheet of local diabetes studies for which I now qualified. One that caught my family and my eyes was the JDRF-funded CLVer study at Stanford University that sought to extend the honeymoon phase of recently diagnosed T1D children through the use of a widely available blood pressure medication called verapamil. As a T1D child who was just entering the honeymoon phase, a time when the pancreas continues to produce significant amounts of insulin, my family and I chose to commit to commuting over an hour each way to the Stanford lab around a dozen times over the course of the next year.
During my extended hospital stay, I learned all about my diagnosis from how my pancreas decided to indefinitely go on strike to why that black and white table on the back of food boxes is actually really important. Between seeing the diabetes educator, endocrinologist, and amazing nurses, I met a JDRF rep who gave me a care package of everything a newly diagnosed T1D teen may need. Most notably, a teddy bear with highlighted fur of where I should and should not stick needles into myself. Also included in the JDRF care package was a reference sheet of local diabetes studies for which I now qualified. One that caught my family and my eyes was the JDRF-funded CLVer study at Stanford University that sought to extend the honeymoon phase of recently diagnosed T1D children through the use of a widely available blood pressure medication called verapamil. As a T1D child who was just entering the honeymoon phase, a time when the pancreas continues to produce significant amounts of insulin, my family and I chose to commit to commuting over an hour each way to the Stanford lab around a dozen times over the course of the next year.
The decision to participate in the study was one of the best T1D-related decisions I have made since diagnosis. The doctors, researchers, and nurses at Stanford are all truly amazing. They are extremely knowledgeable, compassionate, and, as an added bonus, many sport similar Dexcoms or Omnipods to my own.
The study randomized me to take 3 pills a night which may have been the placebo or the real verapamil drug which the CLVer study was testing. Dr. Bruce Buckingham, the researcher in charge and doctor with whom I worked most closely throughout the trial, was especially helpful in helping me manage the responsibilities of volunteering in the study and developing a better understanding of my new life with diabetes.
 Since then, I continue my life as a teenager, making my way through school, swim team, and water polo with very few diabetes related obstacles. Despite my diagnosis, I have adapted to live a very successful and happy life with my friends and family and look forward to continuing to self manage this ‘‘disease.” I am very grateful for the support my doctors and family have given me in allowing me to live my best life.
Since then, I continue my life as a teenager, making my way through school, swim team, and water polo with very few diabetes related obstacles. Despite my diagnosis, I have adapted to live a very successful and happy life with my friends and family and look forward to continuing to self manage this ‘‘disease.” I am very grateful for the support my doctors and family have given me in allowing me to live my best life.
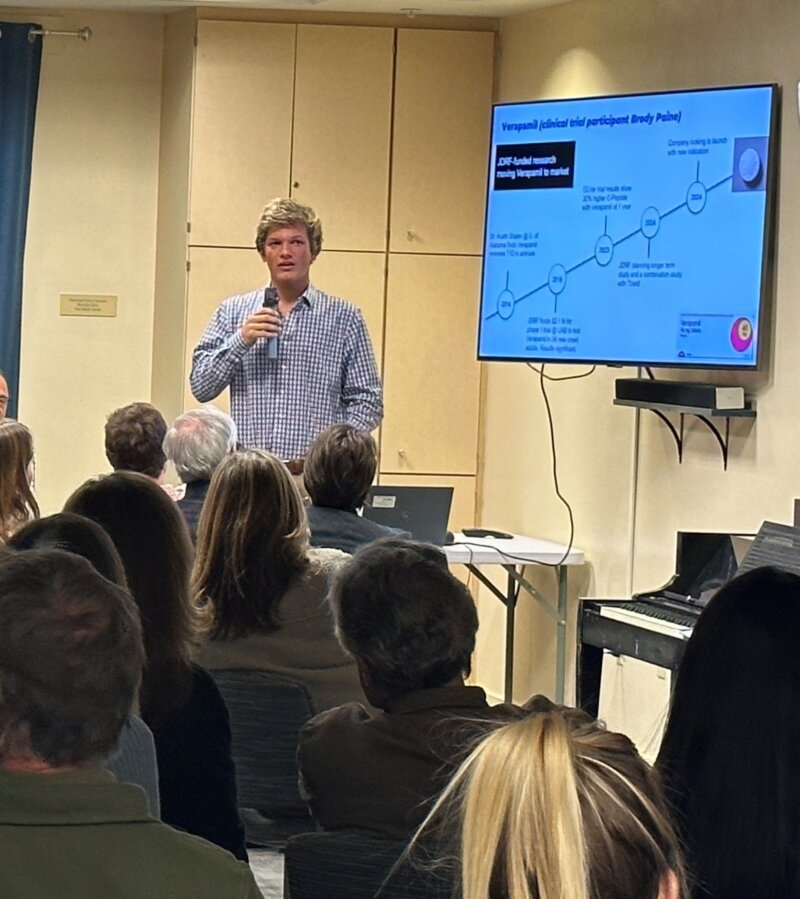
Thanks to participating in the CLVer study, which recently proved verapamil very effective in helping recently diagnosed juvenile diabetics manage sugar levels, I lived my life under the guidance of Dr. Bruce Buckingham, one of the best doctors in the field, and his elite team. Since the original study concluded and results were published, my primary endocrinologist prescribed me verapamil and I continue to participate in a 5 year continuation study with Stanford, albeit with much less commitment. I am extremely grateful that I was able to give back to the diabetic community through volunteering in a study and highly recommend the process to any diabetic looking for ways to contribute to our community.
There are lots of opportunities to participate in a clinical trial in the Northern California area and beyond as well as remotely. Click here to learn more and sign up.