Insulin Injection Techniques and Tips
 People with type 1 diabetes (T1D) manage the disease through insulin therapy. Insulin can be administered through multiple daily injections (MDI) or via an insulin pump.
People with type 1 diabetes (T1D) manage the disease through insulin therapy. Insulin can be administered through multiple daily injections (MDI) or via an insulin pump.
Multiple daily insulin injections come in the form of long-acting (basal) and short-acting (bolus). Long-acting insulin is meant to mimic the body’s natural insulin production throughout the day. Short-acting, or rapid, insulin is administered before eating and to correct high blood-sugar levels. The number of daily injections varies from person to person.
Injection Options and Tips
Syringes and insulin pens are both options for injecting insulin. Some people find insulin pens to be more convenient when they only need a single kind of insulin. Some children also find pen needles are more comfortable than syringe needles.
For both syringes and insulin pens, these general guidelines can make the process easier:
- Always be sure to wash your hands or use hand sanitizer before injecting insulin to reduce the risk of site infection.
- Use a fresh needle for each injection. Sharp needles cause the least amount of trauma to the skin.
- Choose the thinnest and shortest needle possible.
- Inject your insulin at room temperature. Cold insulin can sting.
- Relax the muscles in the area you are injecting. This helps make the nerves less sensitive when you inject into the fat. If you have limited body fat, pinching the area where you will inject insulin can make it easier.
Using a Syringe to Inject Insulin
- Gather supplies
- Insulin vial – at room temperature (roll the vial if pre-mixed insulin or NPH)
- Syringe
- Alcohol swab
- Sharps container – to dispose of the syringe
- Wash your hands or use hand sanitizer
- Prepare the Syringe
- Remove the cap from the syringe and fill it with air equal to the amount of insulin you plan to inject. (i.e. If you plan to inject 2 units, draw the syringe back to 2 units.)
- Stick the needle of the syringe into the vial and inject the air into the bottle.
- With the needle still inside, turn the insulin vial upside down.
- Pull on the plunger of the syringe to draw the correct amount of insulin. Line up the top of the plunger with the correct line.
- Tap the side of the syringe to allow any bubbles to float to the top. Push any bubbles out of the syringe with the plunger and withdraw the plunger back so the syringe fills with insulin to the correct dose.
- Remove the needle from the bottle.
- Inject the Insulin
- Choose an injection site where you have fatty tissue such as the belly, top of the thigh, back of the arm, side of the hips or buttocks area. Rotate the site every time you inject.
- Pinch up the skin and push the needle straight into the skin all the way in at a 90-degree angle.
- Push the plunger down and let go of the pinch. Hold the needle in place for 5 seconds.
- Dispose of the syringe in a sharps container.
Using an Insulin Pen to Inject Insulin
1. Prepare the Insulin Pen
- Roll the pen (Only necessary if pre-mixed or NPH)
- Put on the pen needle. Remove outer and inner caps.
- Dial the pen to 2 units. Do a 2 unit “air shot” or priming the pen (You may need to do it more than once if you do not see insulin come out.)
- Dial the pen to the dose you need.
2. Inject the Insulin
- Choose an injection site where you have fatty tissue such as the belly, top of the thigh, back of the arm, side of the hips or buttocks area. Rotate the site every time you inject.
- Pinch up the fatty area and push the needle straight into the skin all the way in at a 90-degree angle.
- Press and hold the button with your thumb. Keep holding button for 5 seconds after the whole amount has gone in. Let go of the pinch.
- Carefully take off the pen needle and put it in the sharps container. Replace the outer cap of the pen.
Safely Disposing of Needles
To safely dispose of needles, you’ll first need to find out the recommended process in your state. Many local health departments or fire stations have a needle disposal program. To find out, call Safe Needle Disposal at 1-800-643-1643 or visit them online.
Remember to never throw loose needles in the garbage!
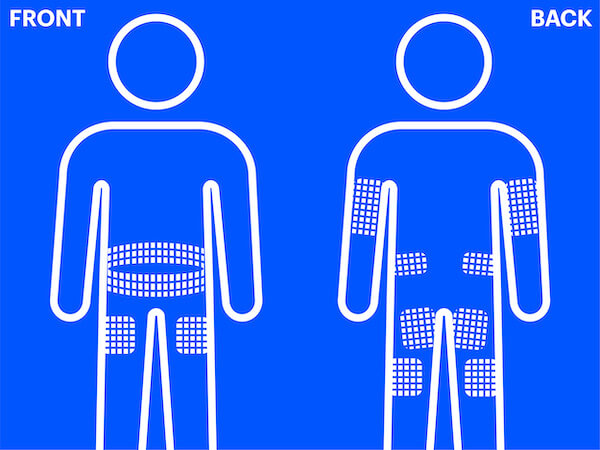
Injection Sites
Injection sites include the stomach (except for 2 inches near the belly button), the top and outer thighs, and upper and outer arms. It is important to not use the same injection site repeatedly to avoid issues such as lipohypertrophy (read more below) or infection. This is also referred to as rotating insulin injection sites.
Lipohypertrophy
Lipohypertrophy occurs if multiple injections are administered to roughly the same part of the skin repeatedly. The skin becomes lumpy and, if insulin is injected into the lumpy area, it won’t be absorbed consistently. If insulin is absorbed too slowly, high blood sugar (hyperglycemia) may occur. If insulin is absorbed too quickly, low blood sugar (hypoglycemia) may occur.
To avoid lumpy skin developing, make sure you pick a different area of skin to put each injection into (rotating your injection site). Ideally, you should aim to keep each new insulin injection spot at least an inch away from your previous injection sites.
Overcoming Fear of Needles
If you are fearful of needles or injections, you’re not alone. Most children have this fear and 1 in 4 adults do as well.
Keep in mind that the insulin injection is given into the fatty skin tissue, which has very few nerve endings. Also, insulin needles are very short and thin. The pain itself, if any, is minimal. Oftentimes it is the anticipation of the injection that causes the most anxiety.
There are devices available that hide the syringe and needle, such as Inject-Ease®, devices to block pain signals, such as ShotBlocker® and Buzzy®, as well as numbing creams like lidocaine or Emla.
You can also explore other insulin delivery options, such as an insulin pump or inhaled insulin.
As always, be sure to speak with your healthcare provider about your fears—they will often have tips and strategies for conquering them!
Young Children and Injections
You may feel stress about giving your young child an insulin injection…and your child may feel stress about getting an insulin injection. Here are some tips on making the process easier:
- First, practice on yourself with an insulin needle and saline solution. It’s important that you build confidence when giving injections.
- Children pick up on your feelings. Remaining calm and confident will help your child feel safe and relaxed.
- Involve your child in the process. Ask them where they’d like the injection. Have them hand you the alcohol wipe and the insulin pen.
- Setting up a reward system, such as a sticker chart, is a great way to reinforce insulin injections as a positive experience.
- Lastly, connect with other families that have children with T1D. A supportive community can help you and your child through the stress and fear you may be experiencing.
How you manage your type 1 diabetes is a personal decision that should be made by you and your healthcare team. JDRF content is for informational purposes only and is not a substitute for professional medical advice. Please contact your doctor or other qualified health provider with any questions you may have regarding type 1 diabetes or any medical condition.
This content was created in collaboration with our partners at the T1D Toolkit.
Injection technique resources are made possible in part through the support of